A groundbreaking study reveals that while the new drug lecanemab successfully removes amyloid buildup, the brain’s crucial waste-disposal system remains damaged, highlighting the complex battle against this neurodegenerative disease.
For decades, the fight against Alzheimer’s disease has been laser-focused on a single, notorious villain: a sticky protein called amyloid-β. The theory, known as the amyloid hypothesis, has been the dominant force in research, suggesting that if we could just clear these protein clumps, or plaques, from the brain, we could halt or even reverse the disease’s devastating cognitive decline. The recent approval of drugs like lecanemab, which do an impressive job of removing amyloid, felt like a monumental victory in this long war. But as with any complex battle, the first victory often reveals a new, more intricate challenge on the horizon.
A new study from researchers at Osaka Metropolitan University in Japan has delivered a dose of sobering reality. While confirming that lecanemab effectively clears amyloid plaques, their findings show it fails to repair a critical piece of underlying machinery: the brain’s own waste-clearance system. This discovery doesn’t diminish the importance of anti-amyloid drugs, but it forces us to look beyond the plaques and confront the deeper, more persistent damage that Alzheimer’s inflicts.
The Brain’s Unsung Janitor: The Glymphatic System
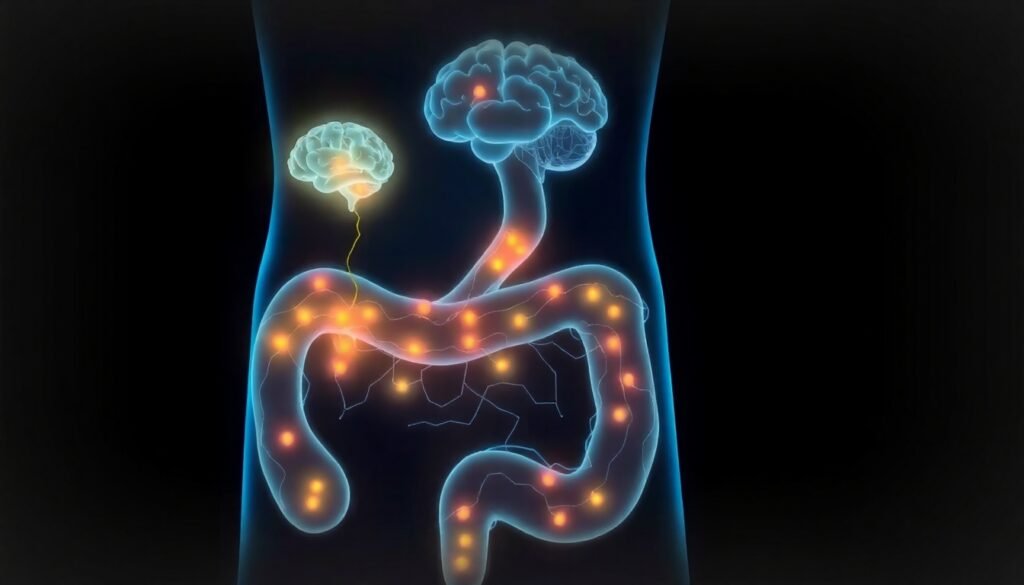
To understand the study’s significance, we first need to appreciate one of the brain’s most elegant and essential processes: the glymphatic system. Think of it as the brain’s dedicated, overnight cleaning crew. While we sleep, this network circulates clear cerebrospinal fluid along the outside of arteries and pushes it deep into brain tissue. There, it mixes with the fluid surrounding our brain cells, collecting metabolic waste products—including stray amyloid-β proteins—before being flushed out of the brain.
This process, managed by glial cells (the “g” in “glymphatic”), is vital for maintaining a healthy neural environment. In a young, healthy brain, the glymphatic system works efficiently, preventing the buildup of toxic debris. It’s a perfect, self-cleaning mechanism that keeps our most important organ running smoothly. However, in Alzheimer’s disease, this finely tuned system begins to break down.
A Vicious Cycle of Damage
As Alzheimer’s disease takes hold, amyloid-β proteins begin to accumulate faster than the glymphatic system can clear them. These proteins form the infamous plaques that stiffen the walls of the brain’s arteries. This stiffening, in turn, cripples the pulsing action of the arteries that helps drive the flow of cerebrospinal fluid. The result is a biological traffic jam. The cleaning fluid can no longer circulate effectively, and waste clearance grinds to a halt.
This creates a devastating feedback loop. Impaired clearance leads to more amyloid buildup, which causes more arterial stiffness, which further impairs clearance. All the while, the accumulating toxic proteins trigger inflammation and damage nearby neurons, leading to the progressive memory loss and cognitive decline that are the hallmarks of Alzheimer’s. By the time symptoms become noticeable, this cycle has been churning away for years, causing significant and widespread damage to the brain’s fundamental infrastructure.
Putting a New Drug to the Test
This is where the new antibody therapy, lecanemab, enters the picture. It’s designed to act like a highly specific magnet, targeting and removing the amyloid-β plaques. The hope was that by removing the primary roadblock, the brain’s glymphatic system might have a chance to recover and get back to its cleaning duties.
To investigate this, a research team led by graduate student Tatsushi Oura and Dr. Hiroyuki Tatekawa designed a focused experiment. They used a specialized MRI technique, known as the Diffusion Tensor Image Analysis along the Perivascular Space (DTI-ALPS) index, to measure the functionality of the glymphatic system in Alzheimer’s patients. This index essentially tracks the movement of water molecules in the spaces around blood vessels, providing a proxy for how well the waste-clearance system is working. The team measured the DTI-ALPS index in patients before they started lecanemab treatment and again three months after therapy began.

A Clean House with Broken Plumbing
The results were both expected and surprising. As anticipated, lecanemab did its job of reducing amyloid levels. However, the DTI-ALPS index showed no significant improvement. Three months into treatment, the patients’ glymphatic systems remained just as impaired as they were before the plaques were cleared.
This finding suggests that simply removing the amyloid plaques isn’t enough to fix the broken plumbing. The long-term damage caused by the disease—the stiffened arteries and compromised fluid dynamics—doesn’t just disappear when the plaques are gone. While drugs like lecanemab can slow cognitive decline by removing a major source of toxicity, they may not be able to restore the brain’s natural resilience on their own, at least not in the short term.
This underscores a critical, evolving understanding of Alzheimer’s: it is not a single-problem disease. It’s a cascade of interconnected failures. By the time a patient is diagnosed, the damage is multifaceted, and a single-target therapy may only address one piece of a much larger puzzle.
The Path Forward: A Multi-Pronged Attack
This research is not a setback but a crucial clarification. It helps explain why even successful anti-amyloid treatments provide modest, rather than miraculous, benefits. The next frontier in Alzheimer’s therapy will likely involve a multi-pronged approach: combining plaque-clearing drugs like lecanemab with other treatments aimed at healing the brain’s underlying systems.
As researcher Tatsushi Oura explained, "Even when Aβ is reduced by lecanemab, impairment of the glymphatic system may not recover within the short-term." The team plans to continue their work, exploring how factors like a patient’s age, the stage of their disease, and other existing damage might influence the glymphatic system’s potential for recovery. "This will help understand the best way to administer treatment to patients," Oura added.
Ultimately, this study refines our map of the Alzheimer’s landscape. It shows us that while we’ve cleared a major obstacle, the road to true recovery is longer and requires us to look deeper. The future of treatment lies not just in cleaning the brain, but in finding ways to repair its fundamental systems and restore its ability to heal itself.
Reference
Oura, T., Tatekawa, H., et al. (2025). Short-term impact of lecanemab on glymphatic system function in Alzheimer’s disease. Journal of Magnetic Resonance Imaging. (Note: Full publication details are pending; this reference is based on the preliminary research announcement.)