A recent study in mice reveals that senescent immune cells in the brain’s white matter could be a key driver of age-related neuroinflammation, opening new doors for therapeutic strategies.
As we age, our bodies undergo a multitude of changes, and the brain is no exception. Many people experience subtle shifts in cognitive function, from slower recall to a general sense of "brain fog." For decades, neuroscientists have sought to understand the precise cellular mechanisms that drive these age-related changes. A groundbreaking new study in mice has illuminated a critical piece of this puzzle, pointing to a specific type of cell that, upon entering a zombie-like state, may be responsible for fanning the flames of chronic brain inflammation.
The research focuses on microglia, the resident immune cells of the central nervous system. Think of them as the brain’s dedicated housekeepers, security guards, and first responders all rolled into one. In a healthy young brain, microglia are constantly patrolling, clearing away cellular debris, pruning unused synaptic connections, and defending against pathogens. They are essential for maintaining a stable and functional neural environment. These cells are particularly important in the brain’s white matter—the vast network of nerve fibers that act as the information superhighways connecting different brain regions.
However, as the brain ages, these once-diligent guardians can change. The new study highlights a phenomenon known as cellular senescence. Senescence is a process where a cell permanently stops dividing but doesn’t die. Instead, it enters a state of suspended animation, earning it the popular moniker of a "zombie cell." While cellular senescence can be beneficial in certain contexts, such as preventing the proliferation of cancerous cells, the accumulation of these senescent cells over time is increasingly linked to a host of age-related diseases, from arthritis to atherosclerosis.

What makes these zombie cells particularly troublesome is their tendency to secrete a cocktail of inflammatory molecules, a phenomenon known as the Senescence-Associated Secretory Phenotype (SASP). This toxic brew can spread to neighboring healthy cells, creating a state of chronic, low-grade inflammation. In the body, this contributes to tissue degradation and dysfunction. The question neuroscientists have been asking is: what happens when this process occurs in the delicate, intricate environment of the brain?
This is where the new research provides a crucial insight. The study, conducted on aging mice, discovered that microglia located specifically within the white matter are susceptible to becoming senescent. As these white matter microglia aged, a significant portion of them transformed into these inflammatory zombie cells. This transformation had a profound effect on the brain’s environment.
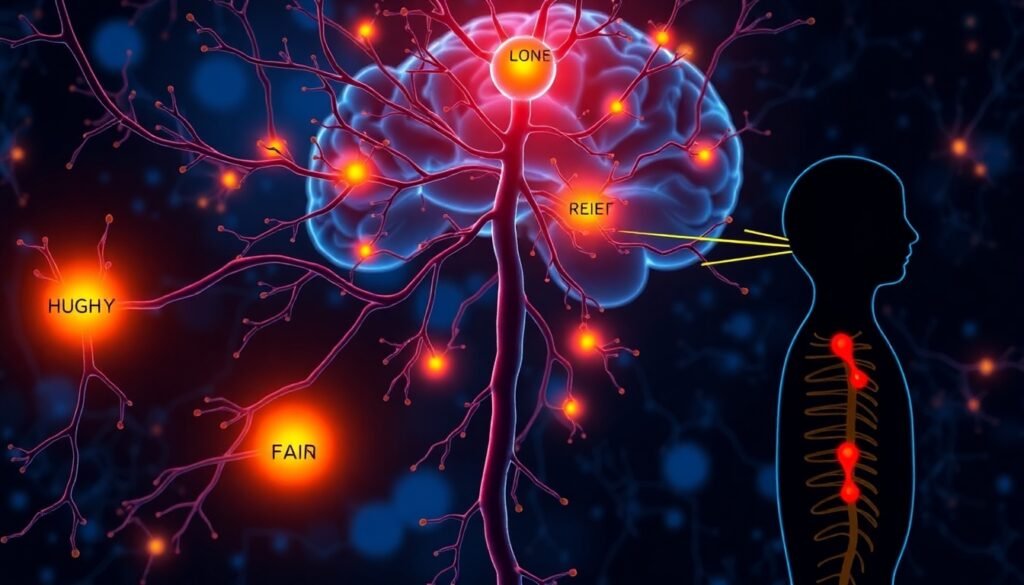
The researchers found that the presence of these senescent microglia significantly exacerbated the brain’s neuroinflammatory phenotype. In other words, they didn’t just stop performing their duties; they actively promoted a harmful, inflammatory state. This chronic inflammation in the white matter is particularly concerning because it can damage myelin, the protective sheath that insulates nerve fibers and ensures the rapid transmission of electrical signals. Damage to myelin can disrupt communication between brain regions, leading to the cognitive and motor deficits associated with aging and neurodegenerative diseases like multiple sclerosis.
The study’s findings suggest a vicious cycle: aging leads to the emergence of senescent microglia, which then release inflammatory signals, creating a toxic environment that can further damage the brain and accelerate the aging process. While this research was conducted in mice, it provides a compelling model for what might be happening in the human brain as we get older.
Perhaps the most exciting aspect of this discovery is the potential for new therapeutic interventions. If the accumulation of senescent microglia is a key driver of age-related neuroinflammation and cognitive decline, then targeting these cells could be a powerful strategy to promote healthy brain aging. This opens the door to the field of senolytics—a class of drugs designed to selectively identify and eliminate senescent cells from the body.
By clearing out these inflammatory zombie cells, senolytic therapies could potentially quell the chronic inflammation in the aging brain, protect the integrity of the white matter, and preserve cognitive function. While the prospect of a pill to reverse brain aging is still in the realm of science fiction, this study provides a concrete biological target. Future research will need to confirm that these same mechanisms are at play in humans and to develop senolytic drugs that can safely and effectively cross the blood-brain barrier to reach their targets.
In conclusion, this research shifts our understanding of brain aging. It’s not just about neurons wearing out; it’s an active process influenced by the brain’s own immune system. By identifying senescent white matter microglia as key culprits in promoting neuroinflammation, scientists have uncovered a new avenue for developing treatments aimed at enhancing brain resilience and extending our years of healthy cognitive function.
Reference
Matsudaira, T., Nakano, S., Konishi, Y., et al. (2025). Cellular senescence in white matter microglia is induced during ageing in mice and exacerbates the neuroinflammatory phenotype. Communications Biology, 8, Article 1531. https://doi.org/10.1038/s42003-025-09139-9