A groundbreaking study reveals a distinct link between the bacteria in our mouths and the progression of MS, opening doors for new diagnostic tools and treatments.
For years, the gut microbiome has been the celebrity of the microbial world. We’ve been told that the trillions of bacteria in our digestive tract hold sway over everything from our mood to our immune system. But what if another bustling microbial metropolis, one much closer to home, plays a critical role in complex neurological diseases? Researchers are now turning their attention to the mouth, and what they’re finding could fundamentally change our understanding of multiple sclerosis (MS).

A pioneering study from the University of Iowa Health Care has provided the most detailed picture yet of the oral microbiome in people with MS. The findings are striking: the community of bacteria, fungi, and viruses living in the mouths of MS patients is significantly different from that of healthy individuals. This research suggests that the key to understanding, and perhaps one day treating, this debilitating autoimmune disease might be found in our saliva.
An Ecosystem in Disarray
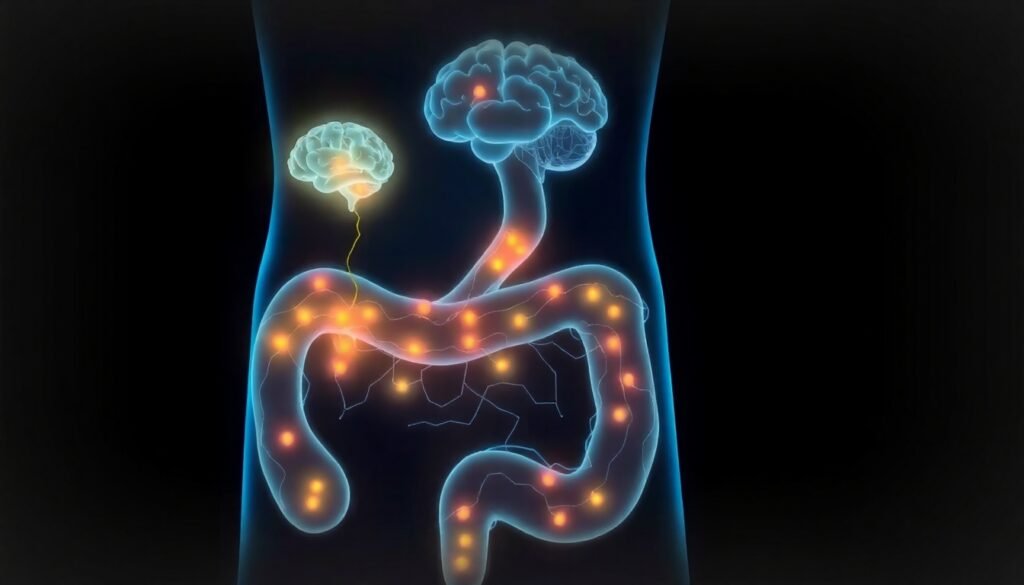
Multiple sclerosis is a progressive disease where the body’s own immune system mistakenly attacks the protective myelin sheath that covers nerve fibers in the brain and spinal cord. This damage disrupts communication between the brain and the rest of the body, leading to a wide range of symptoms, including muscle weakness, vision problems, and cognitive difficulties. While the gut microbiome has long been implicated in the immune dysregulation seen in MS, the oral microbiome has remained largely unexplored—until now.
“While the gut microbiome has long been linked to MS, the oral microbiome, our mouth’s rich microbial ecosystem, has received far less attention,” explains Dr. Ashutosh Mangalam, a professor of pathology at the University of Iowa and the senior author of the study. He notes that the mouth contains the second most diverse microbiome in the human body and has already been connected to other conditions like Alzheimer’s disease and rheumatoid arthritis.
Using state-of-the-art techniques like shotgun metagenomic sequencing and untargeted metabolomics, Dr. Mangalam’s team analyzed saliva samples from 50 individuals with relapsing-remitting MS (the most common form) and 50 healthy controls. Their analysis revealed a clear state of dysbiosis—a microbial imbalance—in the MS patients. It wasn’t just a minor shift; it was a fundamental breakdown of the oral ecosystem.
The Good, The Bad, and The Missing
The research painted a detailed picture of this breakdown. In the mouths of MS patients, there was a significant loss of beneficial “early colonizer” bacteria. These microbes, such as Streptococcus and Actinomyces, are like the foundation of a healthy oral community, creating a stable environment for other good bacteria to thrive. Their absence creates a vacuum.
Filling that void was an influx of bacteria known for their potential to cause inflammation and disease. The study found an enrichment of microbes like Fusobacterium nucleatum, Porphyromonas gingivalis, and several Prevotella species. These are often associated with periodontal disease and are known to provoke inflammatory responses—a critical factor in an autoimmune disease like MS.
“This isn’t just about losing a few good bacteria; it suggests a there is a breakdown of the oral ecosystem in people with MS,” Dr. Mangalam adds. This shift from a cooperative, healthy community to one dominated by inflammatory agents could be a key contributor to the systemic inflammation that drives MS pathology.
To dig deeper, the researchers employed a novel machine-learning method called topic modeling. This allowed them to identify entire communities of bacteria that normally coexist. The analysis showed that five distinct microbial networks present in healthy individuals were significantly depleted or completely lost in MS patients, confirming that the disruption was widespread and systematic.
A Missing Molecule and a Telltale Signature
The study went beyond just identifying the bacteria; it also analyzed the metabolic byproducts in the saliva. This revealed another crucial piece of the puzzle: people with MS had significantly lower levels of a protective metabolite called hypotaurine.
Hypotaurine is a powerful molecule involved in antioxidant defense and maintaining nerve health. Its job is to protect cells from oxidative stress, a form of cellular damage implicated in many neurodegenerative diseases, including MS. The researchers suggest that the reduced levels of hypotaurine are likely a direct consequence of the altered oral microbiome. The loss of beneficial bacteria that may produce or support hypotaurine levels, combined with the rise of inflammatory microbes, creates a double blow to the body’s protective mechanisms.
This distinct microbial and metabolic signature in the saliva of MS patients is a landmark discovery. It provides one of the most detailed views to date of the intricate relationship between oral microbes, their function, and the host’s metabolism in the context of MS.
A New Horizon for Diagnostics and Treatment
While there is currently no cure for MS, these findings open up exciting new possibilities for how we diagnose, monitor, and treat the disease. The implications could be transformative for patients.
First, the discovery of a unique oral signature could lead to the development of simple, non-invasive diagnostic tools. A saliva test is far easier and less uncomfortable for patients than a spinal tap or MRI. Such a test could potentially be used to detect MS earlier, monitor disease activity, or even track a patient’s response to treatment by observing changes in their oral microbiome and metabolite levels.
Second, and perhaps most exciting, is the potential for new therapeutic strategies. The oral microbiome is much more accessible and easier to manipulate than the gut microbiome. This could pave the way for a new class of MS treatments focused on restoring a healthy oral ecosystem. Imagine targeted probiotics, prebiotics, or other therapies designed to reintroduce beneficial bacteria and suppress the inflammatory ones. By rebalancing the oral microbiome, it might be possible to reduce systemic inflammation and slow the progression of the disease.
This research powerfully expands our understanding of MS beyond the traditional focus on the brain and gut, highlighting the mouth as another critical site of immune-microbial interaction. As Dr. Mangalam puts it, “Your mouth may reveal more about your overall health than you think.” For those living with MS, that revelation may hold the promise of a healthier future.
Reference
Fitzjerrells, R., Aguilar Meza, L., Yadav, M., Olalde, H., Paullus, M., Hoang, J., Cherwin, C., Cho, T., Brown, G., Ganesan, S. M., & Mangalam, A. (2024). Multiple sclerosis patients exhibit oral dysbiosis with decreased early colonizers and lower hypotaurine level. npj Biofilms and Microbiomes, 10(1), 48. https://doi.org/10.1038/s41522-024-00514-z